Abstract
Background: Dietary guidelines recommend increasing fruit and vegetable intake and, most recently, have also suggested increasing variety.
Objective: We prospectively examined the independent roles of quantity and variety in fruit and vegetable intake in relation to incident coronary heart disease (CHD).
Design: We prospectively followed 71,141 women from the Nurses’ Health Study (1984–2008) and 42,135 men from the Health Professionals Follow-Up Study (1986–2008) who were free of diabetes, cardiovascular diseases, and cancer at baseline. Diet was assessed by using a validated questionnaire and updated every 4 y. Variety was defined as the number of unique fruit and vegetables consumed at least once per week. Potatoes, legumes, and fruit juices were not included in our definition of fruit and vegetables.
Results: During follow-up, we documented 2582 CHD cases in women and 3607 cases in men. In multivariable analyses, after adjustment for dietary and nondietary covariates, those in the highest quintile of fruit and vegetable intake had a 17% lower risk (95% CI: 9%, 24%) of CHD. A higher consumption of citrus fruit, green leafy vegetables, and β-carotene– and vitamin C–rich fruit and vegetables was associated with a lower CHD risk. Conversely, quantity-adjusted variety was not associated with CHD.
Conclusions: Our data suggest that absolute quantity, rather than variety, in fruit and vegetable intake is associated with a significantly lower risk of CHD. Nevertheless, consumption of specific fruit and vegetable subgroups was associated with a lower CHD risk.
INTRODUCTION
Of the several dietary factors implicated in coronary heart disease (CHD)4 prevention, the evidence is most consistent for fruit and vegetables (1, 2). Dietary recommendations have repeatedly underscored the value of increasing intakes of fruit and vegetables in the diet, and, most recently, have also highlighted the importance of greater variety. For example, the most recent American Heart Association diet and lifestyle guidelines for cardiovascular disease risk reduction have issued a recommendation to consume a variety of fruit and vegetables (3). Likewise, the 2010 Dietary Guidelines for Americans emphasize the importance of increased fruit and vegetable intake and greater variety (4).
In a few cross-sectional studies, higher variety scores for fruit and vegetable intake were associated with lower odds of the metabolic syndrome, obesity, hypercholesterolemia, and hypertension (5, 6). However, these studies did not entirely separate the concept of variety from quantity, because those with greater variety also had greater intakes of fruit and vegetables. Therefore, it is not clear whether the observed associations for variety were independent of quantity of consumption. We previously reported on the association of fruit and vegetable intake with risk of CHD over 8–14 y of follow-up and observed that for every one serving greater intake of fruit and vegetables per day, risk of CHD was lower by 4% (7). The primary objective of this study was to examine the independent associations of quantity and variety in fruit and vegetable intake in relation to incident CHD over a longer period of time in the Nurses’ Health Study (NHS) and the Health Professionals Follow-Up Study (HPFS).
SUBJECTS AND METHODS
Study population
The NHS was initiated in 1976 as a prospective cohort study of 121,701 female registered nurses, 30–55 y of age, from 11 US states. The HPFS is a prospective cohort study of 51, 529 male health professionals, 40–75 y of age, from all 50 states that began in 1986. In both cohorts, information on medical history, lifestyle, potential risk factors, and disease diagnosis, were updated every 2 y with the use of validated questionnaires (8, 9).
For the current investigation, we excluded participants with incomplete dietary assessments or with previously diagnosed cancer, diabetes, or cardiovascular disease at baseline (1984 for NHS, 1986 for HPFS).We also excluded women who left ≥10 items blank on the food-frequency questionnaire (FFQ) or those with implausible energy intakes (<500 or >3500 kcal/d). Men who left ≥70 items blank on the FFQ or who reported daily energy intake outside the plausible range of 800 to 4200 calories were also excluded. We also excluded participants without baseline information on fruit and vegetable intake or follow-up information on CHD diagnosis date (see Supplemental Table S1 under “Supplemental data” in the online issue). The final population consisted of 71,141 women and 42,135 men with complete information. The study was approved by the Human Research Committee of Brigham and Women's Hospital in Boston. All participants gave informed consent.
Ascertainment of diet
Diet was first comprehensively assessed in 1984 in the NHS and in 1986 in the HPFS by using a 126-item semiquantitative FFQ. Therefore, the baseline for the analyses is 1984 for women and 1986 for men. Beginning in 1986, in NHS and HPFS, the FFQ was sent to participants every 4 y to update information on their diet. The reproducibility and validity of these FFQs in measuring food intake have been described previously in detail (10–13). The FFQ asked participants to report their usual intake (never to ≥6 times/d) of a standard portion size (eg, 0.5 cups strawberries, 1 banana, 0.5 cups cooked spinach) of fruit and vegetables. Frequencies and portions for the individual food items were converted to average daily intake of each fruit and vegetable item for each participant. Average daily intakes of individual fruit and vegetable items were summed to compute total fruit and vegetable intake and intakes of fruit and vegetable subgroups. Definitions of the various subgroups (citrus fruit, green leafy vegetables, cruciferous vegetables, and fruit and vegetables rich in β-carotene, lutein, lycopene, or vitamin C) were adapted from our previous study (7) and a study by Steinmetz et al (14) and are presented as supplemental data (see Supplemental Table S2 under “Supplemental data” in the online issue). We did not include potatoes, soy, or other legumes in our definition of vegetables. Because, the American Heart Association does not consider fruit juice to be equivalent to whole fruit (3), fruit juice was not included in our analyses. Variety in fruit and vegetable intake was defined as the total number of unique fruit and vegetables consumed at least once per week. To account for minor differences in the number of fruit and vegetable items assessed at each follow-up cycle, we standardized our variety score to 30 (11 for fruit score and 19 for vegetable score).
Ascertainment of endpoint
The primary endpoint for this study was nonfatal myocardial infarction or fatal CHD occurring after the return of the 1984 FFQ but before 1 June 2008 in women and after return of the 1986 questionnaire but before 1 January 2008 in men. Participants (or next of kin for deceased) reporting a primary endpoint were asked for permission to have their medical records reviewed by physicians who were blinded to the participant's risk factor status. Myocardial infarction was confirmed by using the WHO criteria of typical symptoms plus either elevated enzymes or diagnostic electrocardiogram changes (15). Infarctions that required hospital admission and for which confirmatory information was obtained by interview or letter, but for which no medical records were available, were classified as probable. We included all confirmed (n = 4757) and probable (n = 1432) cases because results were similar when probable cases were excluded.
Deaths were identified by reports from next of kin, the US postal system, or by using certificates obtained from state vital statistics departments and the National Death Index. Follow-up for deaths was >98% complete (16). Fatal CHD was categorized as “definite” only if confirmed by hospital record or autopsy report or if CHD was listed as the cause of death on the death certificate and there was evidence of previous coronary disease. If no medical records were available, we categorized persons in whom CHD was the underlying cause on the death certificate as “presumed” cases.
Data analysis
We evaluated the individual associations between variety and total quantity in fruit and vegetable intake in relation to CHD risk. Fruit and vegetable intake and the variety score were highly correlated (NHS and HPFS: r = 0.68, P < 0.001). Inclusion of both variables in a regression model may introduce multicollinearity and may artificially inflate the variance around the point estimate. We, therefore, regressed the variety score on the total amount of fruit and vegetable intake to estimate the variation in variety score that is independent of total quantity. We then evaluated the independent associations between residuals in variety score (quantity-adjusted fruit and vegetable variety score) with CHD.
Person-time was calculated from the return of the baseline questionnaire to the first CHD event (fatal CHD or nonfatal myocardial infarction), death, loss to follow-up, or the cutoff date (1 June 2008 in NHS and 31 January 2008 in HPFS), whichever occurred first. Each participant contributed only one endpoint and the cohort at risk of each 2-y follow-up period included only those who remained free of CHD at the beginning of each follow-up period. Participants who reported a diagnosis of cancer, cardiovascular disease, or diabetes or had a coronary artery surgery before completion of the baseline dietary questionnaires were excluded. Because of differences in sex, follow-up time, and the questionnaires in the 2 cohorts, all analyses were performed separately in each cohort to achieve better control of confounding. For the primary analyses, to obtain overall estimates for both sexes and to increase statistical power, the RRs from the age and multivariable-adjusted models from the 2 cohorts were combined with the use of an inverse variance-weighted meta-analysis by the fixed-effects model (17).
Within each cohort, participants were divided into quintiles of cumulatively averaged quantity and quantity-adjusted variety in fruit and vegetable intake to reduce within-person variation and best represent long-term intake. The lowest quintile formed the reference category. Cumulative averages were computed by calculating the mean servings per day and variety from all available FFQs up to the beginning of a follow-up interval. Median values of intake for each of the quintiles were used to test for a linear trend across the quintiles. Cubic splines with 4 kn were used to test for nonlinearity.
Cox proportional hazard models with time-varying covariates with age as the time scale were used for all analyses. In our multivariable model, we adjusted for several well established confounders of the association between diet and CHD. These include BMI, smoking status (never, past, or current 1–14, 14–25, or ≥25 cigarettes/d), physical activity (<3.0, 3.0–8.9, 9.0–17.9, 18.0–26.9, or ≥27.0 metabolic equivalents/wk), menopausal status (premenopausal, postmenopausal with no history of hormone therapy, or postmenopausal with current hormone therapy), parental history of early myocardial infarction (defined as infarction before age 65 y for a participant's mother or before age 55 y for a participant's father), multivitamin use (yes or no), aspirin use (yes or no), and alcohol intake (g/d). Because components of dietary patterns can confound the association between diet and disease (18), we also adjusted for several dietary covariates, including total energy intake (kcal/d), intakes of trans fatty acids (g/d), cereal fiber (g/d), red meat (servings/d), and fish (servings/d). For each 2-y time period, we updated information on all nondietary covariates to account for changes in risk factors over time. For dietary covariates, we used the cumulative average of food intakes from baseline to the censoring events to best represent long-term diet and minimize within-person variation (19, 20). Because the diagnosis of intermediate outcomes, including angina, coronary artery surgery or angioplasty, hypercholesterolemia, hypertension, or diabetes in a follow-up cycle resulted in a subsequent change in fruit and vegetable intake (data not shown), we stopped updating diet at the beginning of the interval in which they had the intermediate outcome (19, 20). We did not include the diagnoses of these intermediate outcomes in our multivariate models as these may all be considered intermediate outcomes on the causal pathway between diet and CHD. To test the robustness of our results, we performed a number of sensitivity analyses. First, we continued updating diet through follow-up but censored participants with a coronary artery procedure or those who had a diagnosis of diabetes. We also included hypertension and hypercholesterolemia as covariates in our model. Second, to test whether our results were biased by stopping updating selectively, we examined the association between baseline diet and risk of CHD in both cohorts. Finally, we tested for potential effect modification by age, smoking status, multivitamin use, and presence of diabetes, hypertension, and hypercholesterolemia.
RESULTS
Baseline characteristics
During 24 and 22 y of follow-up in the NHS and HPFS, respectively, we documented 2582 incident cases of CHD among women and 3607 incident cases among men. Higher intakes of fruit and vegetables were associated with several healthy lifestyle characteristics at baseline, including, lower rates of smoking, higher rates of multivitamin use, higher physical activity, higher fruit and vegetable variety score, and higher intakes of cereal fiber and fish (Table 1). Quantity was positively associated with age. Participants with a higher quantity-adjusted variety score were less likely to smoke, were more physically active, and had higher intakes of fruit and vegetables, trans fatty acids, fish, and cereal fiber. Women with higher variety were more likely to be multivitamin and aspirin users (Table 2). Compared with the participants in the main cohort, women included in the current analysis were similar in age, BMI, and physical activity levels. However, there were more women in the current analysis who were current smokers, had hypertension, and had hypercholesterolemia. On the other hand, compared with men in the main cohort, men in the current analysis were slightly younger and were more physically active. There were also fewer men who had hypertension or hypercholesterolemia (see Supplemental Table S3 under “Supplemental data” in the online issue).
TABLE 1.
Age-standardized cardiovascular disease risk factors by baseline quintiles of fruit and vegetable intake in 71,141 women and 42,135 men1
| Women (n =1984) |
Men (n =1986) |
|||||||||
| Q1 | Q2 | Q3 | Q4 | Q5 | Q1 | Q2 | Q3 | Q4 | Q5 | |
| Median intake (servings/d) | 2.25 | 3.38 | 4.35 | 5.49 | 7.59 | 2.14 | 3.28 | 4.29 | 5.52 | 7.83 |
| Participants (n) | 14,232 | 14,218 | 14,234 | 14,227 | 14,230 | 8426 | 8422 | 8433 | 8427 | 8427 |
| Age (y) | 48.6 ± 7.02 | 49.5 ± 7.1 | 50.2 ± 7.1 | 50.8 ± 7.1 | 51.7 ± 7.0 | 51.3 ± 9.2 | 52.5 ± 9.4 | 53.2 ± 9.5 | 53.7 ± 9.6 | 54.7 ± 9.7 |
| BMI (kg/m2) | 24.8 ± 4.7 | 24.9 ± 4.5 | 24.9 ± 4.6 | 24.9 ± 4.5 | 25.0 ± 4.7 | 25.0 ± 5.1 | 24.9 ± 5.0 | 25.0 ± 4.7 | 24.8 ± 4.9 | 24.8 ± 5.1 |
| Current smoker (%) | 33 | 27 | 23 | 20 | 17 | 13 | 10 | 8 | 7 | 5 |
| Family history of MI (%) | 19 | 19 | 19 | 19 | 20 | 30 | 32 | 32 | 32 | 33 |
| Hypertension (%) | 19 | 20 | 20 | 20 | 21 | 19 | 19 | 20 | 19 | 20 |
| Hypercholesterolemia (%) | 7 | 7 | 7 | 8 | 9 | 9 | 10 | 10 | 11 | 12 |
| Current hormone use (%) | 22 | 23 | 25 | 26 | 26 | |||||
| Multivitamin use (y) | 33 | 35 | 37 | 40 | 42 | 30 | 31 | 33 | 33 | 36 |
| Aspirin use at least once per week (%) | 70 | 71 | 72 | 72 | 70 | 26 | 26 | 27 | 27 | 26 |
| Physical activity (MET-h/wk) | 10.2 ± 17.2 | 12.2 ± 20.4 | 13.6 ± 17.4 | 15.6 ± 20.4 | 19.5 ± 26.9 | 15.7 ± 22.2 | 18.2 ± 24.4 | 21.0 ± 30.8 | 23.5 ± 31.4 | 29.1 ± 36.9 |
| Dietary factors | ||||||||||
| Alcohol (g/d) | 7.0 ± 12.1 | 7.1 ± 11.6 | 7.0 ± 10.9 | 6.9 ± 10.6 | 6.7 ± 10.6 | 12.1 ± 16.5 | 12.1 ± 16.0 | 11.5 ± 15.6 | 10.9 ± 14.3 | 10.3 ± 13.9 |
| Energy (kcal/d) | 1460 ± 466 | 1622 ± 471 | 1739 ± 483 | 1856 ± 499 | 2064 ± 538 | 1682 ± 529 | 1858 ± 553 | 1975 ± 567 | 2124 ± 595 | 2358 ± 644 |
| Variety score3 | 5.3 ± 2.8 | 9.0 ± 3.1 | 11.4 ± 3.4 | 13.5 ± 3.6 | 16.4 ± 4.0 | 4.7 ± 2.7 | 8.3 ± 3.0 | 10.6 ± 3.3 | 12.9 ± 3.6 | 16.1 ± 4.2 |
| Red meat (servings/d) | 1.1 ± 0.7 | 1.1 ± 0.7 | 1.2 ± 0.7 | 1.2 ± 0.7 | 1.1 ± 0.7 | 1.2 ± 0.8 | 1.2 ± 0.8 | 1.2 ± 0.8 | 1.2 ± 0.8 | 1.0 ± 0.9 |
| trans Fat (g/d) | 3.4 ± 1.6 | 3.7 ± 1.7 | 3.8 ± 1.7 | 3.9 ± 1.8 | 3.9 ± 1.8 | 2.8 ± 1.5 | 2.9 ± 1.6 | 2.9 ± 1.6 | 2.9 ± 1.6 | 2.8 ± 1.6 |
| Fish (servings/d) | 0.2 ± 0.2 | 0.2 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.2 | 0.4 ± 0.3 | 0.2 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.3 | 0.4 ± 0.3 | 0.5 ± 0.4 |
| Cereal fiber (g/d) | 4.0 ± 2.5 | 4.1 ± 2.4 | 4.2 ± 2.3 | 4.2 ± 2.3 | 4.2 ± 2.2 | 5.3 ± 3.8 | 5.7 ± 3.7 | 6.0 ± 4.0 | 6.0 ± 3.6 | 6.3 ± 4.3 |
Data are age-standardized except for age. MET-h, metabolic equivalent task hours; MI, myocardial infarction; Q, quintile.
Mean ± SD (all such values).
Variety score is defined as the number of unique fruit and vegetables consumed at least once per week.
TABLE 2.
Age-standardized cardiovascular disease risk factors by baseline quintiles of quantity-adjusted fruit and vegetable variety in 71,141 women and 42,135 men1
| Women (n = 1984) |
Men (n =1986) |
|||||||||
| Q1 | Q2 | Q3 | Q4 | Q5 | Q1 | Q2 | Q3 | Q4 | Q5 | |
| Participants (n) | 14,228 | 14,228 | 14,229 | 14,228 | 14,228 | 8427 | 8426 | 8429 | 8426 | 8427 |
| Age (y) | 50.4 ± 7.22 | 49.9 ± 7.2 | 49.9 ± 7.2 | 50.0 ± 7.1 | 50.5 ± 7.1 | 53.9 ± 9.7 | 53.3 ± 9.5 | 52.8 ± 9.5 | 52.6 ± 9.5 | 52.8 ± 9.3 |
| BMI (kg/m2) | 24.8 ± 4.7 | 24.7 ± 4.6 | 24.9 ± 4.6 | 24.9 ± 4.6 | 25.0 ± 4.6 | 24.9 ± 5.2 | 24.9 ± 5.1 | 25.0 ± 4.7 | 24.9 ± 4.9 | 24.9 ± 5.1 |
| Current smoker (%) | 27 | 25 | 24 | 22 | 22 | 10 | 9 | 8 | 8 | 7 |
| Family history of MI (%) | 19 | 19 | 19 | 19 | 19 | 32 | 32 | 32 | 31 | 32 |
| Hypertension (%) | 21 | 20 | 20 | 20 | 20 | 20 | 20 | 19 | 19 | 19 |
| Hypercholesterolemia (%) | 8 | 8 | 8 | 7 | 8 | 10 | 10 | 10 | 10 | 11 |
| Current hormone use (%) | 24 | 24 | 25 | 25 | 25 | |||||
| Multivitamin use (y) | 36 | 36 | 37 | 38 | 40 | 33 | 32 | 32 | 32 | 33 |
| Aspirin use at least once per week (%) | 69 | 71 | 71 | 73 | 72 | 27 | 27 | 27 | 26 | 27 |
| Physical activity (MET-h/wk) | 13.4 ± 22.1 | 13.4 ± 20.5 | 14.0 ± 19.8 | 14.9 ± 21.0 | 15.6 ± 21.1 | 21.2 ± 34.7 | 20.0 ± 27.1 | 21.1 ± 27.3 | 21.8 ± 31.0 | 23.1 ± 29.0 |
| Dietary factors | ||||||||||
| Alcohol (g/d) | 7.3 ± 12.2 | 7.3 ± 11.8 | 7.0 ± 11.2 | 6.7 ± 10.6 | 6.3 ± 9.7 | 11.2 ± 15.8 | 11.4 ± 15.9 | 11.5 ± 15.3 | 11.3 ± 14.8 | 11.2 ± 14.5 |
| Energy (kcal/d) | 1638 ± 554 | 1707 ± 522 | 1756 ± 523 | 1796 ± 510 | 1845 ± 517 | 1878 ± 642 | 1927 ± 606 | 2003 ± 605 | 2062 ± 607 | 2123 ± 612 |
| Fruit and vegetables (servings/d) | 4.3 ± 3.4 | 4.0 ± 2.2 | 4.3 ± 2.0 | 4.7 ± 1.8 | 5.0 ± 1.7 | 4.6 ± 3.9 | 4.2 ± 2.3 | 4.5 ± 2.2 | 4.9 ± 2.0 | 5.4 ± 1.9 |
| Red meat (servings/d) | 1.1 ± 0.7 | 1.2 ± 0.7 | 1.2 ± 0.7 | 1.2 ± 0.7 | 1.1 ± 0.7 | 1.1 ± 0.8 | 1.2 ± 0.8 | 1.2 ± 0.8 | 1.2 ± 0.8 | 1.2 ± 0.8 |
| trans Fat (g/d) | 3.5 ± 1.7 | 3.7 ± 1.7 | 3.8 ± 1.8 | 3.8 ± 1.7 | 3.9 ± 1.7 | 2.6 ± 1.6 | 2.8 ± 1.6 | 2.9 ± 1.6 | 3.0 ± 1.6 | 2.9 ± 1.5 |
| Fish (servings/d) | 0.2 ± 0.3 | 0.3 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.3 | 0.3 ± 0.3 | 0.3 ± 0.3 | 0.3 ± 0.3 | 0.4 ± 0.3 |
| Cereal fiber (g/d) | 4.1 ± 2.6 | 4.1 ± 2.4 | 4.1 ± 2.3 | 4.2 ± 2.2 | 4.2 ± 2.2 | 5.7 ± 4.4 | 5.9 ± 4.3 | 5.9 ± 3.7 | 5.9 ± 3.6 | 5.9 ± 3.4 |
Data are age-standardized except for age. Variety score is defined as the number of unique fruit and vegetables consumed at least once per week. Quantity-adjusted variety score was calculated by regressing fruit and vegetable intake (servings/d) on fruit and vegetable variety score. MET-h, metabolic equivalent task hours; MI, myocardial infarction; Q, quintile.
Mean ± SD (all such values).
Regression analysis
In pooled multivariable-adjusted analyses, higher intakes of fruit and vegetables were significantly associated with lower risk of CHD (RR for highest quintile: 0.83; 95% CI: 076, 0.91). Similarly, higher intakes of the various subgroups, including all fruit (RR for highest quintile: 0.88; 95% CI: 0.80, 0.96), all vegetables (RR for highest quintile: 0.89; 95% CI: 0.81, 0.97), citrus fruit (RR for highest quintile: 0.91; 95% CI: 0.84, 0.99), green leafy vegetables (RR for highest quintile: 0.83; 95% CI: 0.77, 0.91), β-carotene–rich foods (RR for highest quintile: 0.84; 95% CI: 0.77, 0.92), and vitamin C–rich foods (RR for highest quintile: 0.85; 95% CI: 0.78, 0.92) were associated with a lower CHD risk (Table 3). For total fruit and vegetables, the risk of CHD was 18% (95% CI: 11%, 24%) lower in the third quintile (∼4 servings/d) compared with the first quintile, and higher intakes were not associated with further decreases in risk. We examined whether the significant associations with certain fruit and vegetable subgroups were due to chance. In the NHS, we found significant statistical heterogeneity in the association of fruit and vegetable subgroups with CHD (P < 0.01). However, in the HPFS, this association was more marginal (P < 0.1). We found no significant association between quantity-adjusted fruit and vegetable variety score and risk of CHD (RR for highest quintile: 1.05; 95% CI: 0.97, 1.13).
TABLE 3.
RRs (95% CIs) for coronary heart disease according to quintiles of quantity and variety in fruit and vegetable intake1
| Q1 | Q2 | Q3 | Q4 | Q5 | P-trend2 | |
| All fruit and vegetables | ||||||
| Women | ||||||
| Servings/d3 | 2.25 | 3.38 | 4.35 | 5.49 | 7.59 | |
| Cases/person-years | 612/315,704 | 517/316,515 | 463/316,845 | 469/316,977 | 521/316,683 | |
| Age-adjusted4 | 1.0 | 0.79 (0.71, 0.89) | 0.67 (0.60, 0.76) | 0.65 (0.58, 0.73) | 0.67 (0.60, 0.76) | <0.0001 |
| Multivariable5 | 1.0 | 0.88 (0.78, 0.99) | 0.78 (0.69, 0.89) | 0.78 (0.69, 0.89) | 0.81 (0.70, 0.93) | 0.004 |
| Men | ||||||
| Servings/d3 | 2.14 | 3.29 | 4.29 | 5.52 | 7.83 | |
| Cases/person-years | 746/161,974 | 715/162,594 | 679/162,911 | 699/162,860 | 768/162,627 | |
| Age-adjusted4 | 1.0 | 0.87 (0.79, 0.97) | 0.78 (0.70, 0.87) | 0.77 (0.69, 0.85) | 0.78 (0.71, 0.86) | <0.0001 |
| Multivariable5 | 1.0 | 0.93 (0.84, 1.04) | 0.85 (0.76, 0.95) | 0.84 (0.75, 0.94) | 0.84 (0.75, 0.95) | 0.007 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.84 (0.78, 0.91) | 0.73 (0.67, 0.79) | 0.72 (0.66, 0.77) | 0.73 (0.68, 0.79) | <0.0001 |
| Multivariable5 | 1.0 | 0.91 (0.84, 0.98) | 0.82 (0.76, 0.89) | 0.82 (0.75, 0.89) | 0.83 (0.76, 0.91) | <0.0001 |
| Fruit | ||||||
| Women | ||||||
| Servings/d3 | 0.44 | 0.91 | 1.35 | 1.85 | 2.84 | |
| Cases/person-years | 623/317,555 | 494/315,140 | 485/315,526 | 439/317,968 | 541/316,535 | |
| Age-adjusted4 | 1.0 | 0.75 (0.67, 0.85) | 0.69 (0.61, 0.77) | 0.57 (0.51, 0.65) | 0.64 (0.57, 0.72) | <0.0001 |
| Multivariable5 | 1.0 | 0.88 (0.78, 0.99) | 0.86 (0.76, 0.97) | 0.77 (0.67, 0.87) | 0.87 (0.76, 0.99) | 0.02 |
| Men | ||||||
| Servings/d3 | 0.42 | 0.89 | 1.35 | 1.93 | 3.07 | |
| Cases/person-years | 704/162,360 | 711/162,789 | 688/162,304 | 697/162,778 | 807/162,736 | |
| Age-adjusted4 | 1.0 | 0.92 (0.83, 1.02) | 0.80 (0.72, 0.89) | 0.74 (0.66, 0.82) | 0.77 (0.70, 0.85) | <0.0001 |
| Multivariable5 | 1.0 | 1.00 (0.90, 1.11) | 0.91 (0.82, 1.01) | 0.85 (0.76, 0.95) | 0.88 (0.78, 0.99) | 0.008 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.84 (0.78, 0.91) | 0.75 (0.69, 0.81) | 0.66 (0.61, 0.72) | 0.71 (0.66, 0.77) | <0.0001 |
| Multivariable5 | 1.0 | 0.94 (0.87, 1.02) | 0.89 (0.82, 0.96) | 0.81 (0.75, 0.89) | 0.88 (0.80, 0.96) | 0.001 |
| Vegetables | ||||||
| Women | ||||||
| Servings/d3 | 1.49 | 2.25 | 2.90 | 3.69 | 5.14 | |
| Cases/person-years | 606/315,781 | 512/316,432 | 457/316,923 | 483/316,906 | 524/316,683 | |
| Age-adjusted4 | 1.0 | 0.84 (0.74, 0.94) | 0.72 (0.64, 0.82) | 0.74 (0.66, 0.84) | 0.76 (0.68, 0.86) | <0.0001 |
| Multivariable5 | 1.0 | 0.89 (0.79, 1.01) | 0.79 (0.70, 0.90) | 0.84 (0.74, 0.96) | 0.85 (0.74, 0.97) | 0.03 |
| Men | ||||||
| Servings/d3 | 1.38 | 2.13 | 2.81 | 3.65 | 5.22 | |
| Cases/person-years | 748/161,889 | 722/162,640 | 703/162,847 | 711/162,897 | 723/162,692 | |
| Age-adjusted4 | 1.0 | 0.94 (0.85, 1.04) | 0.90 (0.81, 0.99) | 0.88 (0.80, 0.98) | 0.87 (0.78, 0.96) | 0.006 |
| Multivariable5 | 1.0 | 0.99 (0.89, 1.09) | 0.96 (0.87, 1.07) | 0.96 (0.86, 1.07) | 0.92 (0.82, 1.03) | 0.13 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.89 (0.83, 0.96) | 0.82 (0.76, 0.88) | 0.82 (0.76, 0.89) | 0.82 (0.76, 0.89) | <0.0001 |
| Multivariable5 | 1.0 | 0.94 (0.87, 1.02) | 0.89 (0.82, 0.96) | 0.91 (0.83, 0.98) | 0.89 (0.81, 0.97) | 0.01 |
| Citrus fruit | ||||||
| Women | ||||||
| Servings/d3 | 0.02 | 0.12 | 0.21 | 0.43 | 0.86 | |
| Cases/person-years | 678/311087 | 502/331,629 | 408/309,328 | 450/309,160 | 544/321,519 | |
| Age-adjusted4 | 1.0 | 0.82 (0.73, 0.92) | 0.67 (0.59, 0.75) | 0.69 (0.62, 0.78) | 0.71 (0.63, 0.79) | <0.0001 |
| Multivariable5 | 1.0 | 0.89 (0.80, 1.01) | 0.81 (0.72, 0.92) | 0.87 (0.77, 0.99) | 0.89 (0.79, 1.00) | 0.26 |
| Men | ||||||
| Servings/d3 | 0 | 0.14 | 0.21 | 0.50 | 1.00 | |
| Cases/person-years | 563/110073 | 1146/273,402 | 429/109,551 | 656/163,489 | 813/156,451 | |
| Age-adjusted4 | 1.0 | 0.91 (0.82, 1.01) | 0.84 (0.74, 0.96) | 0.76 (0.68, 0.85) | 0.85 (0.76, 0.94) | 0.005 |
| Multivariable5 | 1.0 | 0.96 (0.86, 1.06) | 0.94 (0.82, 1.06) | 0.83 (0.74, 0.93) | 0.92 (0.83, 1.03) | 0.14 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.87 (0.81, 0.94) | 0.75 (0.69, 0.82) | 0.73 (0.67, 0.79) | 0.78 (0.72, 0.84) | <0.0001 |
| Multivariable5 | 1.0 | 0.93 (0.86, 1.00) | 0.87 (0.80, 0.96) | 0.85 (0.78, 0.92) | 0.91 (0.84, 0.99) | 0.07 |
| Green leafy vegetables | ||||||
| Women | ||||||
| Servings/d3 | 0.22 | 0.50 | 0.72 | 1.00 | 1.50 | |
| Cases/person-years | 642/313303 | 510/313,701 | 448/323,425 | 491/318,239 | 491/314,056 | |
| Age-adjusted4 | 1.0 | 0.78 (0.69, 0.87) | 0.68 (0.60, 0.76) | 0.68 (0.61, 0.77) | 0.69 (0.61, 0.77) | <0.0001 |
| Multivariable5 | 1.0 | 0.81 (0.72, 0.91) | 0.76 (0.67, 0.86) | 0.77 (0.68, 0.86) | 0.78 (0.69, 0.88) | 0.0004 |
| Men | ||||||
| Servings/d3 | 0.14 | 0.43 | 0.64 | 0.93 | 1.43 | |
| Cases/person-years | 731/142,396 | 899/205,065 | 623/144,839 | 732/169,076 | 622/151,591 | |
| Age-adjusted4 | 1.0 | 0.90 (0.81, 0.99) | 0.87 (0.78, 0.97) | 0.82 (0.74, 0.91) | 0.80 (0.72, 0.89) | <0.0001 |
| Multivariable5 | 1.0 | 0.93 (0.85, 1.03) | 0.93 (0.83, 1.04) | 0.89 (0.80, 0.98) | 0.88 (0.79, 0.99) | 0.02 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.85 (0.78, 0.91) | 0.78 (0.72, 0.84) | 0.76 (0.70, 0.82) | 0.75 (0.69, 0.81) | <0.0001 |
| Multivariable5 | 1.0 | 0.88 (0.81, 0.95) | 0.85 (0.78, 0.92) | 0.83 (0.76, 0.90) | 0.83 (0.77, 0.91) | <0.0001 |
| Cruciferous vegetables | ||||||
| Women | ||||||
| Servings/d3 | 0.14 | 0.28 | 0.39 | 0.56 | 0.92 | |
| Cases/person-years | 564/315288 | 488/327,977 | 503/310,973 | 481/310,190 | 546/318,295 | |
| Age-adjusted4 | 1.0 | 0.91 (0.81, 1.03) | 0.93 (0.82, 1.05) | 0.87 (0.77, 0.99) | 0.94 (0.83, 1.05) | 0.40 |
| Multivariable5 | 1.0 | 0.97 (0.86, 1.10) | 1.00 (0.89, 1.13) | 0.95 (0.84, 1.07) | 1.03 (0.91, 1.17) | 0.64 |
| Men | ||||||
| Servings/d3 | 0.14 | 0.28 | 0.35 | 0.56 | 1.00 | |
| Cases/person-years | 702/151,434 | 784/189,328 | 641/148,941 | 704/159,559 | 776/163,704 | |
| Age-adjusted4 | 1.0 | 0.91 (0.82, 1.00) | 0.92 (0.83, 1.03) | 0.91 (0.82, 1.01) | 0.93 (0.84, 1.02) | 0.41 |
| Multivariable5 | 1.0 | 0.94 (0.85, 1.04) | 0.96 (0.86, 1.07) | 0.96 (0.86, 1.07) | 0.96 (0.86, 1.07) | 0.77 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.91 (0.84, 0.98) | 0.93 (0.86, 1.00) | 0.89 (0.83, 0.97) | 0.93 (0.86, 1.01) | 0.24 |
| Multivariable5 | 1.0 | 0.95 (0.88, 1.03) | 0.98 (0.90, 1.06) | 0.95 (0.88, 1.03) | 0.99 (0.91, 1.07) | 0.96 |
| β-Carotene–rich fruit and vegetables | ||||||
| Women | ||||||
| Servings/d3 | 0.14 | 0.26 | 0.37 | 0.57 | 0.93 | |
| Cases/person-years | 572/310,978 | 589/322,765 | 484/313,975 | 502/318,788 | 435/316,218 | |
| Age-adjusted4 | 1.0 | 0.88 (0.78, 0.98) | 0.78 (0.69, 0.88) | 0.76 (0.67, 0.85) | 0.63 (0.55, 0.71) | <0.0001 |
| Multivariable5 | 1.0 | 0.94 (0.84, 1.06) | 0.90 (0.79, 1.02) | 0.91 (0.80, 1.03) | 0.79 (0.69, 0.90) | 0.0008 |
| Men | ||||||
| Servings/d3 | 0.14 | 0.21 | 0.28 | 0.50 | 0.86 | |
| Cases/person-years | 648/142,829 | 748/168,089 | 735/181,762 | 743/159,932 | 733/160,355 | |
| Age-adjusted4 | 1.0 | 0.94 (0.85, 1.05) | 0.83 (0.75, 0.92) | 0.89 (0.80, 0.98) | 0.82 (0.73, 0.91) | 0.0005 |
| Multivariable5 | 1.0 | 0.99 (0.89, 1.10) | 0.90 (0.80, 1.00) | 0.95 (0.85, 1.06) | 0.88 (0.79, 0.99) | 0.04 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.91 (0.84, 0.98) | 0.81 (0.75, 0.87) | 0.83 (0.76, 0.90) | 0.73 (0.67, 0.79) | <0.0001 |
| Multivariable5 | 1.0 | 0.97 (0.89, 1.05) | 0.89 (0.82, 0.97) | 0.93 (0.86, 1.01) | 0.84 (0.77, 0.92) | 0.0002 |
| Lutein-rich fruit and vegetables | Tertile 1 | Tertile 2 | Tertile 3 | |||
| Women | ||||||
| Servings/d3 | 0.0 | 0.07 | 0.21 | |||
| Cases/person-years | 867/502,389 | 720/484,167 | 995/596,168 | |||
| Age-adjusted4 | 1.0 | 0.90 (0.82, 0.99) | 0.94 (0.86, 1.03) | 0.33 | ||
| Multivariable5 | 1.0 | 0.96 (0.87, 1.06) | 1.01 (0.92, 1.11) | 0.66 | ||
| Men | ||||||
| Servings/d3 | 0.0 | 0.07 | 0.21 | |||
| Cases/person-years | 1171/242,771 | 1101/235,560 | 1335/334,635 | |||
| Age-adjusted4 | 1.0 | 0.98 (0.90, 1.06) | 0.89 (0.82, 0.96) | 0.003 | ||
| Multivariable5 | 1.0 | 1.01 (0.93, 1.10) | 0.94 (0.87, 1.03) | 0.12 | ||
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.94 (0.89, 1.01) | 0.91 (0.86, 0.97) | 0.004 | ||
| Multivariable5 | 1.0 | 0.99 (0.93, 1.06) | 0.97 (0.91, 1.03) | 0.36 | ||
| Lycopene-rich fruit and vegetables | ||||||
| Women | ||||||
| Servings/d3 | 0.18 | 0.32 | 0.50 | 0.67 | 1.04 | |
| Cases/person-years | 598/320,593 | 459/315,545 | 545/336,938 | 393/293,008 | 587/316,639 | |
| Age-adjusted4 | 1.0 | 0.83 (0.73, 0.94) | 0.84 (0.74, 0.94) | 0.76 (0.67, 0.87) | 0.94 (0.83, 1.05) | 0.55 |
| Multivariable5 | 1.0 | 0.86 (0.76, 0.98) | 0.88 (0.78, 0.99) | 0.82 (0.72, 0.94) | 0.95 (0.84, 1.07) | 0.72 |
| Men | ||||||
| Servings/d3 | 0.14 | 0.28 | 0.50 | 0.79 | 1.14 | |
| Cases/person-years | 599/134,173 | 786/191,878 | 867/192,928 | 605/134,471 | 750/159,516 | |
| Age-adjusted4 | 1.0 | 1.07 (0.96, 1.19) | 0.98 (0.88, 1.09) | 1.06 (0.94, 1.18) | 1.02 (0.92, 1.14) | 0.94 |
| Multivariable5 | 1.0 | 1.11 (0.99, 1.23) | 1.02 (0.92, 1.14) | 1.10 (0.98, 1.24) | 1.06 (0.95, 1.19) | 0.52 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.96 (0.88, 1.04) | 0.91 (0.84, 0.98) | 0.91 (0.84, 0.99) | 0.98 (0.91, 1.06) | 0.77 |
| Multivariable5 | 1.0 | 0.99 (0.91, 1.08) | 0.95 (0.88, 1.03) | 0.97 (0.89, 1.06) | 1.01 (0.93, 1.09) | 0.76 |
| Vitamin C–rich fruit and vegetables | ||||||
| Women | ||||||
| Servings/d3 | 0.24 | 0.44 | 0.66 | 0.95 | 1.50 | |
| Cases/person-years | 679/325611 | 435/303,174 | 468/321,747 | 484/315,202 | 516/316,990 | |
| Age-adjusted4 | 1.0 | 0.70 (0.62, 0.79) | 0.69 (0.61, 0.78) | 0.70 (0.62, 0.78) | 0.67 (0.59, 0.75) | <0.0001 |
| Multivariable5 | 1.0 | 0.78 (0.69, 0.89) | 0.81 (0.72, 0.91) | 0.86 (0.76, 0.97) | 0.83 (0.73, 0.94) | 0.07 |
| Men | ||||||
| Servings/d3 | 0.21 | 0.42 | 0.71 | 1.06 | 1.72 | |
| Cases/person-years | 751/156,558 | 690/175,010 | 657/149,503 | 730/169,817 | 779/162,078 | |
| Age-adjusted4 | 1.0 | 0.86 (0.77, 0.95) | 0.88 (0.79, 0.98) | 0.80 (0.73, 0.89) | 0.80 (0.73, 0.89) | 0.0001 |
| Multivariable5 | 1.0 | 0.91 (0.82, 1.02) | 0.94 (0.84, 1.04) | 0.88 (0.79, 0.97) | 0.87 (0.78, 0.97) | 0.02 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.79 (0.73, 0.85) | 0.79 (0.73, 0.86) | 0.76 (0.70, 0.82) | 0.74 (0.69, 0.80) | <0.0001 |
| Multivariable5 | 1.0 | 0.86 (0.79, 0.93) | 0.88 (0.81, 0.95) | 0.87 (0.80, 0.94) | 0.85 (0.78, 0.92) | 0.003 |
| Quantity-adjusted variety score7 | ||||||
| Women | ||||||
| Cases/person-years | 541/315,759 | 530/316,340 | 486/316,883 | 486/317,046 | 539/316,695 | |
| Age-adjusted4 | 1.0 | 1.05 (0.93, 1.19) | 0.98 (0.87, 1.11) | 0.96 (0.85, 1.09) | 1.02 (0.91, 1.15) | 0.87 |
| Multivariable5 | 1.0 | 1.12 (0.99, 1.26) | 1.07 (0.95, 1.21) | 1.08 (0.95, 1.22) | 1.12 (0.99, 1.27) | 0.13 |
| Men | ||||||
| Cases/person-years | 839/161,580 | 720/162,371 | 665/162,947 | 672/163,054 | 711/163,014 | |
| Age-adjusted4 | 1.0 | 0.91 (0.83, 1.01) | 0.86 (0.78, 0.95) | 0.87 (0.79, 0.96) | 0.92 (0.83, 1.01) | 0.05 |
| Multivariable5 | 1.0 | 0.96 (0.86, 1.06) | 0.94 (0.84, 1.04) | 0.95 (0.86, 1.05) | 1.01 (0.91, 1.11) | 0.99 |
| Pooled6 | ||||||
| Age-adjusted4 | 1.0 | 0.97 (0.89, 1.04) | 0.91 (0.84, 0.98) | 0.91 (0.84, 0.98) | 0.96 (0.89, 1.03) | 0.11 |
| Multivariable5 | 1.0 | 1.02 (0.94, 1.10) | 0.99 (0.91, 1.07) | 1.00 (0.92, 1.08) | 1.05 (0.97, 1.13) | 0.34 |
Q, quintile.
Median values of the exposure for each category were used to test for a linear trend across categories.
Median values are for quintiles of fruit and vegetable intake (servings/d).
Adjusted for age (y).
Multivariable models were adjusted for age (y), calendar year, BMI (10 categories), total energy intake (quintiles of kcal), smoking status (never, past, or current 1–14, current 15–24, or current ≥25 cigarettes/d), physical activity (<3.0, 3–8.9, 9.0–17.9, 18.0–26.9, or ≥27.0 metabolic equivalents/wk), menopausal status and postmenopausal hormone use (for women only; premenopausal, postmenopausal with no history of hormone therapy use, postmenopausal with history of hormone therapy use, or postmenopausal with current hormone therapy), alcohol intake (0, 0.1.0–4.9, 5.0–9.9, 10.0–14.9, or ≥15.0 g/d), parental history of early myocardial infarction (before age 65 y for mother or age 55 y for father), multivitamin use (yes or no), and aspirin use (yes or no), and intakes of trans fatty acids (quintiles of g/d), cereal fiber (quintiles of g/d), red meat (quintiles of servings/d), and fish (quintiles of servings/d).
Results were combined with the use of a fixed-effects model.
Quantity-adjusted variety score was calculated by regressing fruit and vegetable intake (servings/d) on fruit and vegetable variety score (number of unique fruit and vegetables consumed at least once per week). All statistical tests were conducted by using Cox proportional hazards regression models.
When we examined nonfatal myocardial infarction and fatal CHD separately, fruit and vegetable intake was significantly associated with nonfatal myocardial infarction (pooled RR for highest quintile: 0.81, 95% CI: 0.72, 0.91) and marginally associated with fatal CHD (pooled RR highest quintile: 0.88, 95% CI: 0.76, 1.02). On the other hand, quantity-adjusted fruit and vegetable variety score was not associated with either nonfatal myocardial infarction (pooled RR for highest quintile: 1.08, 95% CI: 0.93, 1.20) or fatal CHD (pooled RR for highest quintile: 1.01, 95% CI: 0.89, 1.14).
Our results remained robust in several sensitivity analyses. When we continued updating a participant's diet throughout follow-up but censored participants with a coronary artery procedure or a diagnosis of diabetes, and included hypertension and hypercholesterolemia as covariates, the association between fruit and vegetable intake and CHD was similar but somewhat attenuated (pooled RR for highest quintile: 0.90; 95% CI: 0.81, 1.00). When we used baseline diet instead of repeated dietary measures, the association between fruit and vegetable intake and CHD was also attenuated as a result of nondifferential misclassification but remained significant despite the greater misclassification of long-term diet (pooled RR for highest quintile: 0.86; 95% CI: 0.79, 0.94). When we only included confirmed cases of CHD in our analyses, results remained unchanged (pooled RR for highest quintile of fruit and vegetable servings: 0.81; 95% CI: 0.73, 0.90; pooled RR for highest quintile of quantity-adjusted fruit and vegetable variety: 1.04; 95% CI: 0.95, 1.13).
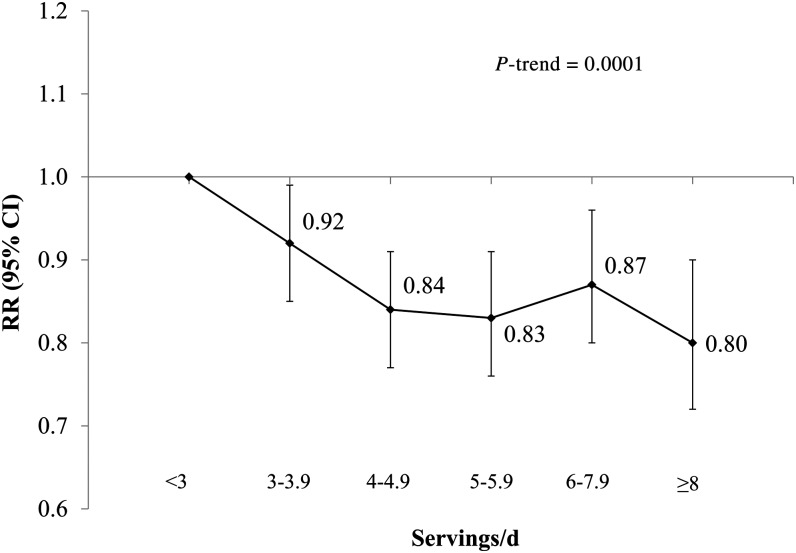
In pooled multivariable analyses, consumption of 4.0 to 4.9 servings/d was associated with a 16% (95% CI: 9%, 23%) lower risk of CHD. Higher intakes were not associated with appreciably lower risks. However, those consuming ≥8 servings/d had the lowest CHD risk (RR: 0.80; 95% CI: 0.72, 0.90, Figure 1). In the NHS, but not HPFS, we found that the association between fruit and vegetable intake and CHD was significantly nonlinear (P for curvature = 0.01; see Supplemental Figure S1 under “Supplemental data” in the online issue). Because the association appeared linear up to ∼5 servings/d, we estimated the risk associated with a linear increase in fruit and vegetable intake for up to 5 servings/d. With each serving of higher fruit and vegetable intake up to 5 servings/d (assessed as a linear trend), the multivariable adjusted RR for CHD was 0.91 (95% CI: 0.87, 0.94).
FIGURE 1.
RRs (95% CIs) for coronary heart disease according to servings of fruit and vegetables in women and men combined. Multivariable RRs were adjusted for age (y), calendar year, BMI (10 categories), total energy intake (quintiles of kcal), smoking status (never, past, and current 1–14, current 15–24, or current ≥25 cigarettes/d), physical activity (<3.0, 3.0–8.9, 9.0–17.9, 18.0–26.9, or ≥27.0 metabolic equivalents/wk), menopausal status and postmenopausal hormone use (for women only; premenopausal, postmenopausal with no history of hormone therapy use, postmenopausal with history of hormone therapy use, or postmenopausal with current hormone therapy), alcohol intake (0, 0.1–4.9, 5.0–9.9, 10.0–14.9, or ≥15.0 g/d), parental history of early myocardial infarction (before age 65 y for mother or age 55 y for father), multivitamin use (yes or no), and aspirin use (yes or no), and intakes of trans fatty acids (quintiles of g/d), cereal fiber (quintiles of g/d), and red meat (quintiles of servings/d), and fish (quintiles of servings/d). Results were combined with the use of a fixed-effects model. All statistical tests were conducted by using Cox proportional hazards regression models. <3.0 servings/d, n = 26,167; 3.0–3.9 servings/d, n = 23,109; 4.0–4.9 servings/d, n = 21,219; 5.0–5.9 servings/d, n = 16,148; 6.0–7.9 servings/d, n = 17,131; ≥8.0 servings/d, n = 9502.
No significant interactions of variety score and fruit and vegetable intake with smoking, multivitamin use, presence of hypertension, hypercholesterolemia, or diabetes mellitus (P-interaction > 0.01 after adjustment for multiple testing) were noted. However, among women, we found a marginal interaction between fruit and vegetable quantity and presence of hypertension (P = 0.02). Fruit and vegetable quantity was significantly associated with risk of CHD among normotensive (RR for highest quintile: 0.71; 95% CI: 0.56, 0.90) but not hypertensive women (RR for highest quintile: 0.92; 95% CI: 0.77, 1.09). The proportional hazards assumption was met and no significant interactions were observed with age.
DISCUSSION
In this prospective cohort study with >20 y of follow-up, we observed that higher quantity, but not variety, in fruit and vegetable consumption was associated with a lower risk of CHD. The inverse association with total quantity was independent of established dietary and nondietary cardiovascular disease risk factors.
Our findings are consistent with those of a meta-analysis of 9 prospective cohort studies in which the risk of CHD decreased by 4% (95% CI: 1%, 7%, P = 0.003) for each additional portion of fruit and vegetable intake (1). Similar to our results, a meta-analysis of 12 cohort studies showed that, relative to <3 servings/d of fruit and vegetables, those consuming >5 servings/d had 17% lower risk of CHD (95% CI: 11%, 23%; P < 0.001) (2). In an earlier analysis within the NHS and the HPFS with 14 and 8 y of follow-up, respectively, each increase in fruit and vegetable servings per day was associated with a 4% lower risk of CHD (95% CI: 1%, 6%) (7). In the current updated analysis with longer follow-up and greater precision in dietary measurement due to repeated dietary measures, each increase of one serving per day in fruit and vegetable intake, overall, was associated with a 3% lower risk of CHD (95% CI: 2%, 5%). Similar to our previous analyses, we observed that the dose-response relation between fruit and vegetable quantity and CHD risk was not entirely linear. Risk appeared to decrease linearly for intakes up to ∼5 servings/d (RR per serving: 0.91; 95% CI: 0.87, 0.94). Higher intakes did not appear to provide additional protection. To our knowledge, only one study examined the association between fruit and vegetable variety, independent of quantity, and CHD. After adjustment for quantity, Oude Griep et al (21) found no association between variety and 10-y incidence of CHD.
The null associations we observed with variety could mean that the putative effects of higher variety on lowering inflammation (22) are not large enough to translate into a lower risk of CHD. It may also be that the FFQ used in our study did not adequately capture variety because it only included, on average, 11 fruit items and 19 vegetable items. The differences in associations of the various fruit and vegetable subgroups with CHD risk may also explain the lack of an association with variety. Because we assigned equal weight to all fruit and vegetables in the variety score, one can increase CHD risk simply by displacing the more protective subgroups with the more neutral ones while keeping total fruit and vegetable intake constant. In addition, fruit and vegetable variety may have been underestimated in some individuals because our FFQ grouped certain fruit into one category (eg, apples or pears; kale, mustard, or chard greens). Finally, it may also be that absolute quantity is more important than higher variety in reducing CHD risk. However, because consumption of various fruit and vegetable subgroups, including citrus fruit, green leafy vegetables, and β-carotene– and vitamin C– rich fruit and vegetables, was significantly associated with a lower CHD risk, a simple and healthful way to increase quantity of consumption is to consume a variety of fruit and vegetables.
Several bioactive components in fruit and vegetables such as carotenoids, vitamin C, fiber, magnesium, and potassium may act synergistically or antagonistically through multiple mechanisms to promote a holistic beneficial effect on CHD risk. Consumption of fruit and vegetables has been shown to protect against the development of type 2 diabetes (23) and metabolic syndrome (24), both of which are known intermediaries and strong risk factors for the development of CHD. Most recently, variety in fruit and vegetable intake, in addition to quantity, was associated with a reduced risk of type 2 diabetes (25). Greater fruit and vegetable variety might allow exposure to a greater range of antioxidants, which may improve markers of endothelial dysfunction (26) and inflammation (27). For example, in a cross-sectional analysis of Puerto Rican adults, those in the highest tertile of fruit and vegetable variety had a 32% lower odds of elevated C-reactive protein compared with participants with the least variety (22). Clinical trials and prospective analyses have consistently shown that diets high in fruit and vegetables reduce the incidence of hypertension, another intermediary in the development of CHD (28, 29). Higher fruit and vegetable consumption is also associated with lower concentrations of total and LDL cholesterol in a dose-response manner (30, 31).
The large sample size, the long follow-up period, and presence of updated dietary and covariate data are unique strengths in our study. In addition, we were able to assess the independent relations of fruit and vegetable quantity and variety with CHD risk. However, our results need to be interpreted in the context of a few limitations. First, participants in our study may be dissimilar to those living in the general population. For example, mean fruit and vegetable intake in our population (4.7 servings/d) was much higher than national estimates (3.0 servings/d) (32). However, the consistency of our findings with previous publications and the existence of strong biological mechanisms make these associations plausible in other population and ethnic groups. Second, although we were able to carefully adjust for known dietary and lifestyle risk factors, residual confounding remains a possibility because of the observational nature of this study. Finally, because diet was self-reported and assessed by FFQs, some measurement error and misclassification was inevitable. However, FFQs used in these studies were validated against multiple diet records (10, 13). Use of repeated measures of diet to calculate cumulative averages would minimize any potential random measurement error caused by within-person variation and would accommodate diet changes over time.
In conclusion, in this large study of US men and women, we found that higher intakes of fruit and vegetables were associated with a lower risk of CHD. Although no associations were observed with variety, the high correlation between variety and quantity combined with our finding that higher intakes of various fruit and vegetable subgroups were associated with lower CHD risk underscores the importance of consuming a varied diet. Public health recommendations and policy efforts should continue to focus on increasing overall quantity and variety in fruit and vegetable intake.
Supplementary Material
Acknowledgments
We are indebted to the participants in the Nurses’ Health Study and Health Professionals Follow-Up Study for their continuing outstanding support and to our colleagues working in these studies for their valuable help.
The authors’ responsibilities were as follows—SNB: designed and conducted the analysis, interpreted the data, and wrote the manuscript; NMW, AP, JEM, KMR, WCW, EBR, and FBH: assisted in interpreting the data and edited the manuscript; JEM, WCW, EBR, and FBH: obtained funding, managed and conducted the Nurses’ Health Study and the Health Professionals Follow-Up Study, and critically reviewed the manuscript for important intellectual content; and FBH: had primary responsibility for the final content. None of the authors had a conflict of interest.
Footnotes
Abbreviations used: CHD, coronary heart disease; FFQ, food-frequency questionnaire; HPFS, Health Professionals Follow-Up Study; NHS, Nurses’ Health Study.
REFERENCES
- 1.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr 2006;136:2588–93. [DOI] [PubMed] [Google Scholar]
- 2.He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens 2007;21:717–28. [DOI] [PubMed] [Google Scholar]
- 3.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006;114:82–96. [DOI] [PubMed] [Google Scholar]
- 4.US Department of Agriculture. Dietary guidelines for Americans, 2010. Washington, DC: US Department of Health and Human Services, 2011.
- 5.Azadbakht L, Mirmiran P, Azizi F. Dietary diversity score is favorably associated with the metabolic syndrome in Tehranian adults. Int J Obes (Lond) 2005;29:1361–7. [DOI] [PubMed] [Google Scholar]
- 6.Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Dietary diversity score and cardiovascular risk factors in Tehranian adults. Public Health Nutr 2006;9:728–36. [DOI] [PubMed] [Google Scholar]
- 7.Joshipura KJ, Hu FB, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, Colditz G, Ascherio A, Rosner B, Spiegelman D, et al. The effect of fruit and vegetable intake on risk for coronary heart disease. Ann Intern Med 2001;134:1106–14. [DOI] [PubMed] [Google Scholar]
- 8.Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Women's Health 1997;6:49–62. [DOI] [PubMed]
- 9.Rimm EB, Giovannucci EL, Willett WC, Colditz GA, Ascherio A, Rosner B, Stampfer MJ. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet 1991;338:464–8. [DOI] [PubMed] [Google Scholar]
- 10.Feskanich D, Rimm EB, Giovannucci EL, Colditz GA, Stampfer MJ, Litin LB, Willett WC. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc 1993;93:790–6. [DOI] [PubMed]
- 11.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 1992;135:1114–26, discussion 27–36. [DOI] [PubMed] [Google Scholar]
- 12.Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, Willett WC. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 1989;18:858–67. [DOI] [PubMed] [Google Scholar]
- 13.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 1985;122:51–65. [DOI] [PubMed] [Google Scholar]
- 14.Steinmetz KA, Potter JD, Folsom AR. Vegetables, fruit, and lung cancer in the Iowa Women's Health Study. Cancer Res 1993;53:536–43. [PubMed] [Google Scholar]
- 15.World Health Organization. IHD Registers: Report of the Fifth Working Group. Copenhagen, Denmark: World Health Organization, 1971. [Google Scholar]
- 16.Stampfer MJ, Willett WC, Speizer FE, Dysert DC, Lipnick R, Rosner B, Hennekens CH. Test of the National Death Index. Am J Epidemiol 1984;119:837–9. [DOI] [PubMed] [Google Scholar]
- 17.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed]
- 18.Imamura F, Lichtenstein AH, Dallal GE, Meigs JB, Jacques PF. Confounding by dietary patterns of the inverse association between alcohol consumption and type 2 diabetes risk. Am J Epidemiol 2009;170:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu FB, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Rosner BA, Hennekens CH, Willett WC. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med 1997;337:1491–9. [DOI] [PubMed] [Google Scholar]
- 20.Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, Willett WC. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol 1999;149:531–40. [DOI] [PubMed] [Google Scholar]
- 21.Oude Griep LM, Verschuren WM, Kromhout D, Ocke MC, Geleijnse JM. Variety in fruit and vegetable consumption and 10-year incidence of CHD and stroke. Public Health Nutr 2012;15:2280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhupathiraju SN, Tucker KL. Greater variety in fruit and vegetable intake is associated with lower inflammation in Puerto Rican adults. Am J Clin Nutr 2011;93:37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ 2010;341:c4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Fruit and vegetable intakes, C-reactive protein, and the metabolic syndrome. Am J Clin Nutr 2006;84:1489–97. [DOI] [PubMed] [Google Scholar]
- 25.Cooper AJ, Sharp SJ, Lentjes MA, Luben RN, Khaw KT, Wareham NJ, Forouhi NG. A prospective study of the association between quantity and variety of fruit and vegetable intake and incident type 2 diabetes. Diabetes Care 2012;35:1293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeon JY, Kim HS, Sung MK. Diets rich in fruits and vegetables suppress blood biomarkers of metabolic stress in overweight women. Prev Med 2012;54(suppl):S109–15. [DOI] [PubMed] [Google Scholar]
- 27.Root MM, McGinn MC, Nieman DC, Henson DA, Heinz SA, Shanely RA, Knab AM, Jin F. Combined fruit and vegetable intake is correlated with improved inflammatory and oxidant status from a cross-sectional study in a community setting. Nutrients 2012;4:29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dauchet L, Czernichow S, Bertrais S, Blacher J, Galan P, Hercberg S. [Fruits and vegetables intake in the SU.VI.MAX study and systolic blood pressure change] Arch Mal Coeur Vaiss 2006;99:669–73 (in French). [PubMed] [Google Scholar]
- 29.Miura K, Greenland P, Stamler J, Liu K, Daviglus ML, Nakagawa H. Relation of vegetable, fruit, and meat intake to 7-year blood pressure change in middle-aged men: the Chicago Western Electric Study. Am J Epidemiol 2004;159:572–80. [DOI] [PubMed] [Google Scholar]
- 30.Djoussé L, Arnett DK, Coon H, Province MA, Moore LL, Ellison RC. Fruit and vegetable consumption and LDL cholesterol: the National Heart, Lung, and Blood Institute Family Heart Study. Am J Clin Nutr 2004;79:213–7. [DOI] [PubMed] [Google Scholar]
- 31.Mirmiran P, Noori N, Zavareh MB, Azizi F. Fruit and vegetable consumption and risk factors for cardiovascular disease. Metabolism 2009;58:460–8. [DOI] [PubMed] [Google Scholar]
- 32.Casagrande SS, Wang Y, Anderson C, Gary TL. Have Americans increased their fruit and vegetable intake? The trends between 1988 and 2002. Am J Prev Med 2007;32:257–63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.